Contact lenses & Covid-19
- Contact lenses will not give you COVID-19. Contact lens wearers should always practice excellent hygiene when wearing lenses. It has been noted that contact lens wearers touch their faces and eyes when inserting and removing lenses. What you need to know is that, touching your face can spread germs.
- Exercise proper hand washing. Wash your hands carefully and thoroughly with soap and water for at least 20 seconds, followed by hand drying with unused paper towels. This should occur before every contact lens insertion and removal. If soap and water are not readily available, use a hand sanitizer that contains at least 60% alcohol. People should avoid touching their face, including their eyes, nose and mouth, with unwashed hands.
- Disinfect contact lenses. Contact lens wearers should either dispose of their daily disposable lenses every evening, or regularly disinfect your monthly and bi weekly lenses according to instructions from the manufacturer.
- Regular Eyeglasses / Spectacles Do Not Provide Protection
No scientific evidence supports rumors that everyday glasses offer protection against COVID-19.
- If you have a contact lens prescription that is nearing expiration or has expired, contact your optician or doctor of optometry. Health professionals are working with patients to ensure they have access to needed medical devices.
- If you are sick, temporarily stop wearing your contacts and use your glasses instead
Once you return to full health and have spoken with your eye doctor, you can start again. Make sure to use new contact lenses and a new lens case.
If you have questions, you can talk to our team for recommendations. To book an appointment for an eye exam to see an optometrist, call us at 905-832-6262.
Our Maple optometrist Location:
Eyes on Eyes Optical
9929 Keele St, Unit 110, Maple, ON L6A 1Y5, Tel: 905-832-6262
Please click here for more information
Eyes on Eyes Optical Store,
Eyes on Eyes Optical is a relatively new store in the Maple region. Owned and operated by Nina Toobaei. With a nursing background, Nina took on the challenge and started studying at Seneca College to become an optician. Nina has been practicing as an Optician since 2005. Nina opened the door to her own optometry, eyes on eyes optical, in the September of 2014.
She started her business with a series of promotions focusing on the needs of the community in Maple. She began with the senior citizens, making sure that every senior citizen could receive a pair of free frames and lenses. Her great promotions and her care and respect for senior citizens brought her publicity in the Maple/Vaughan area. Eyes on Eyes Optical has quickly become Vaughan's go-to optical boutique for custom-made prescription eyewear. They provide fantastic customer service with a mix of different designer eyewear from all significant fashion countries, a huge range of choices, remarkable, breathtaking designer sunglasses, sports goggles, and contact lenses. They introduce you to the latest technology in lenses and coatings. They also offer comprehensive eye exams and contact lens fittings. All under one roof and all at affordable prices! For those of you who have insurance benefits, they provide an online submission. They help to fill the insurance forms and mailing it to the insurance company.
Eyes on Eyes optometry office is equipped for comprehensive eye examination.
Dr. Natalie Saleh graduated from the University of Toronto with a Bachelor of Science degree in Biology. She received her Doctorate of Optometry from the New England College of Optometry in Boston, Massachusetts. Dr. Saleh completed externships at the South Boston Community Health Center in Boston MA, Bascom Palmer Hospital Pediatric Clinic in Miami Fl, VA Hospital in Jamaica Plain, MA and Toronto Eye Clinic and Dr. David Ng and Associates in Toronto, On. She care for the vision needs of families from eye tests to treating compromised vision and eye emergencies. They also offer the convenience of Saturday and evening appointments with our optometrists on site. To book an appointment please call 905-832-6262.
They provide you with the best product at the best value. They take pride in the work and their services. Their staff can help you choose the right glasses, and have them ready for you within the hour to 24 hours in most cases. Eyes on Eyes Optical is equipped with a state of the art laboratory, where they are able to manufacture lenses on-site. This is a place where you find your perfect vision back and they make you their customer forever.
What are Digital lenses?
Digital lenses are made using Digital technology with digital machinery. High-definition lenses are designed to supply sharper and clearer vision in all conditions. The high-definition eyeglass lenses are also called free-form lenses. The term "free-form" refers to an advanced manufacturing process.
The process is based on a digital scanning of every individual eyes. The lenses are customized exactly for your eyes. Digital lens technology, are one of the most important revolution and transformation in prescription eyeglasses.
Digital Lenses practically are six times clearer than old non digital lenses. The production of the lenses is optimized with computer-controlled surfacing equipment that is much more precise than ordinary and traditional tools.
Digital lenses are the best solution to reduce distortion in curved frames. Digital lenses intensify and increase night time and peripheral vision. Issues such as eye strain, headaches, and dizziness can all be lowered to a minimum with digital lenses. People with high prescription needs and astigmatism can also be dispensed with high definition lenses technology.
With digital lenses, patient are less restricted when choosing frame or sunglasses. Therefore, high definition lens technology provides and extends both fashion and function needs. Not only digital prescription lenses are accurate and meticulous, but they also have less distortion on the sides of the lens.
Digital lenses also have the benefit of being individually modify and adjust to suit every patient’s unique needs. Optician or eye doctor will take accurate measurements to customize a lens for every individual unique prescription.
At Eyes on Eyes Optical, we only dispense high quality digital lenses like Nikon, Hoya, Ziess,….
If you need to book an appointment to come and see an optometrist for eye exam, please either call us at 905-832-6262 or you can book an appointment via our website which is eyesoneyesoptical.ca
We have an optometrist in our office every Tuesday afternoon, Thursday morning and Saturday 10.00 to 3.00 pm
Please click here for more info
What is Anisometropia
Anisometropia is an eye condition which the two eyes have unequal power. One eye can be nearsighted or, farsighted or can have a combination of both. This condition is called antimetropia. Generally a difference in power of two diopters or more is the accepted anisometropia.
This condition occurs when your eyes have different refractive powers, that can result your eyes to focus unevenly. Normally Anisometropia occur when the two eye are a different size or different shape than the other. This condition causes unsymmetrical curvatures, unsymmetrical farsightedness, or asymmetric nearsightedness.
One of the most common causes of amblyopia that is also known as Lazy Eye, is Anisometropia.

Causes:
We still do not know completely what the causes of anisometropia are. But having different eye sizes can be a major factor.
Anisometropia influences our binocular vision. Any individual with anisometropia normally see a larger image with one eye and a smaller image with the other eye and causes blurry vision. Therefore, one of the eyes may become weaker than the other that cause the brain to favor the stronger eye. This can cause amblyopia if the anisometropia is not caught and treated early. People with untreated anisometropia may experience symptoms like headaches, nausea, dizziness, visual discomfort and poor depth perception.
Although anisometropia can be present from birth and it is not typically discover until childhood. About 6% of all children between the ages of 5 and 18 suffer from anisometropia.
There are three types of anisometropia:
Simple Anisometropia
This is when one eye is
affected while the other eye has no refractive error. The eye can be either nearsighted or farsighted.
This kind of anisometropia can be treated using spactacles. Simple
anisometropia causes one eye to see a clear image and the other eye sees blurry
image.
Compound Anisometropia
This is when both eyes are
myopic or nearsighted, although there will be a significant difference in their
refractive errors. This causes one eye to see a more blurred image than the
other. This
form of anisometropia causes both eyes to see blurry images, but one eye’s
vision will be significantly blurrier.
Mixed Anisometropia
Mixed anisometropia occurs when both eyes have refractive errors but one is myopic (nearsighted), and the other is hyperopic (farsighted).
Treatment & Management Options
Anisometropia needs to be treated as soon as it is diagnosed. If treatment is delayed the brain may decide to favor the eye that presents a clearer image over the other eye, leading to dependence on the stronger eye. If this occurs, the non-favored eye will become increasingly weaker.
Anisometropia can be treated using a variety of methods, which are determined based on the severity of the condition. Treatments can include corrective lenses, contact lenses, or laser eye surgery. For corrective lenses or contact lenses to be effective they will need to be different prescriptions so that each eye can have its visual needs met.
Individuals with large degrees anisometropia
typically cannot rely on corrective lenses for treatment. Eyeglasses have a
magnifying effect, which can significantly change the size of the image seen by
each eye. As such individuals with large degrees of anisometropia may find that
eyeglasses negatively affect their binocular vision.
If you have questions, you can talk to our team for recommendations. To book an appointment for an eye exam to see an optometrist, call us at 905-832-6262.
Please click here for more info.
Our Maple optometrist Location:
Eyes on Eyes Optical
9929 Keele St, Unit 110, Maple, ON L6A 1Y5, Tel: 905-832-6262
What is Astigmatism?
Astigmatism is a common vision condition that causes blurred vision. It occurs when the cornea (the clear front cover of the eye) is irregularly shaped or sometimes because of the curvature of the lens inside the eye. ... Most people have some degree of astigmatism.
Astigmatism is a refractive error, like farsightedness and nearsightedness, meaning it is not an eye disease; it's just a problem with how the eye focuses light.
In an eye with astigmatism, light fails to come to a single focus on the retina to produce clear vision. Instead, multiple focus points occur, either in front of the retina or behind it (or both).
Astigmatism Symptoms
Astigmatism usually causes blurred or distorted vision to a certain degree at all distances.
Symptoms of uncorrected astigmatism are eye strain and headaches, especially after reading or other prolonged visual tasks.
Squinting also is also a very common telltale sign that one has developed astigmatism.
What Causes Astigmatism?
Astigmatism is caused by an irregularly shaped cornea. Instead of the cornea having a symmetrically round shape (like a baseball), it is shaped more like an American football, with one meridian being more curved than the meridian perpendicular to it.
The steepest and flattest meridians of an eye with astigmatism are called the principal meridians.
In some cases, astigmatism is caused by the shape of the lens inside the eye. This is called lenticular astigmatism, to differentiate it from the more common corneal astigmatism.
Types of Astigmatism
There are three primary types of astigmatism:
- Myopic astigmatism. One or both principal meridians of the eye are nearsighted. (If both meridians are nearsighted, they are myopic in differing degree.)
- Hyperopic astigmatism. One or both principal meridians are farsighted. (If both are farsighted, they are hyperopic in differing degree.)
- Mixed astigmatism. One principal meridian is nearsighted, and the other is farsighted.
Astigmatism can also be known and classified as regular or irregular. In regular astigmatism, the principal meridians are 90 degrees apart (perpendicular to each other). In irregular astigmatism, the principal meridians are not perpendicular. Most astigmatism is regular corneal astigmatism, which gives the front surface of the eye an oval shape.
Irregular astigmatism can result from an eye injury that has caused scarring on the cornea, from certain types of eye surgery or from keratoconus, a disease that causes a gradual thinning of the cornea.
Astigmatism Correction Options
Astigmatism, like nearsightedness and farsightedness, usually can be corrected with eyeglasses, contact lenses or refractive surgery.
If you have questions, you can talk to our team for recommendations. We sell the best lenses and coatings in our Maple Location. To book an appointment for an eye exam to see an optometrist, call us at 905-832-6262.
Our Maple optometrist Location: Eyes on Eyes Optical
9929 Keele St, Unit 110, Maple, ON L6A 1Y5, Tel: 905-832-6262
HOW TO CARE FOR CONTACT LENSES
It is an exciting time for many patients to start using contact lenses instead of glasses. Many patients love the activities they can enjoy without worrying about glasses. Even though there are many benefits of wearing contact lenses, you might be facing a risk of eye infection if you fail to care for the contacts. If you decide to wear contact lenses, you also need to have a pair of glasses as well. Please keep in the mind that contact lenses are not for 24/7. In our office, we provide Contact lens training. If you choose to wear contact lenses, then it is important to follow these tips:
Select Lenses
Do you worry about your diligence to clean and care for your contact lenses every day? If you aren’t consistent with hygiene habits, then you might consider disposable lenses instead of weekly or monthly contacts. With disposable lenses, you don’t need to worry about regular cleaning because the lenses are discarded after they are used.
Clean the Lenses Daily
- Before you touch contact lens, wash and rinse your hands with soap and warm water. ...
- Dry your hands with a clean, lint-free towel.
- If you use hair spray, use it before you put in your contact lens. ...
- Also put on eye makeup after you put in your contact lenses. ...
- Always store the lenses in fresh contact lens solution.
- Never put tap water directly on your lenses. Even distilled water can be home to nasty little bugs that can cause an infection or hurt your vision.
- Never put a contact in your mouth to rinse it.
- Clean each contact this way: Rub it gently with your index finger in the palm of your other hand. Lightly rubbing your contact removes surface buildup.
- Clean your lens case every time you use it. Use either sterile solution or hot tap water. Let it air dry
Do’s and Don’ts with your contact lenses
- Wear your contact lenses each day only as long as your doctor recommends.
- Never wear someone else’s contacts, especially if they’ve already been worn. Using other people's contact lenses can spread infections or particles from their eyes to yours.
- Never wear someone else’s contacts, especially if they’ve already been worn. Using other people's contact lenses can spread infections or particles from their eyes to yours.
- Don’t sleep with your contacts. When your eyelids are closed, your tears don’t bring as much oxygen to your eyes as when they’re open.
- Don't let the tip of solution bottles touch other surfaces, like your fingers, eyes, or contacts. Any of them can contaminate the solution.
- Wear sunglasses with total UV protection when you’re in the sun. Contacts can make your eyes more light-sensitive.
- Use an eye drop or plain saline solution or whatever your doctor recommends -- to keep your eyes moist.
- If you accidentally insert your contacts inside out, don’t worry. It won’t hurt your eye. You can
- If your eye gets irritated, take your contacts out. Don’t use them again until you’ve spoken to someone at your doctor’s office about the problem. If you keep wearing them, your eye could get infected. When you do start to wear contacts again, follow your doctor's instructions to prevent an infection.
- Go to your eye doctor right away if you have any sudden vision loss, blurred vision that doesn’t get better, light flashes, eye pain, infection, swelling, unusual redness, or irritation.
- Don’t swim with your contacts in. Goggles are better than nothing, but there’s still a chance you could get a serious infection if you wear contacts in a pool, or worse, in a lake.
Replace Your Contact Lens Case
Make sure to keep the contact lens case clean. It is a good idea to replace the case every three months. If you need a new contact lens case, then you are welcome to stop by our Maple Optometrist office to get a replacement.
Talk to our opticians to learn the proper replacement timeline for your contact lenses. Don’t make the mistake of wearing the lenses longer than recommended because you will increase the risk of an eye infection.
Regular Eye Exams
Keep in mind that your prescription will change with time. So, it is a good idea to visit your eye doctor annually to get a new prescription. This appointment is a great time for the doctor to examine your eyes and identify any early signs of eye disease.
Is it time for you to visit an eye doctor? Schedule an appointment with our team of optometrists.
Our Maple Optometrist office is located in 9929 Keele street, Maple, L6A 1Y5. To Book for an eye exam or to book for contact lens training, please call 905-832-6262
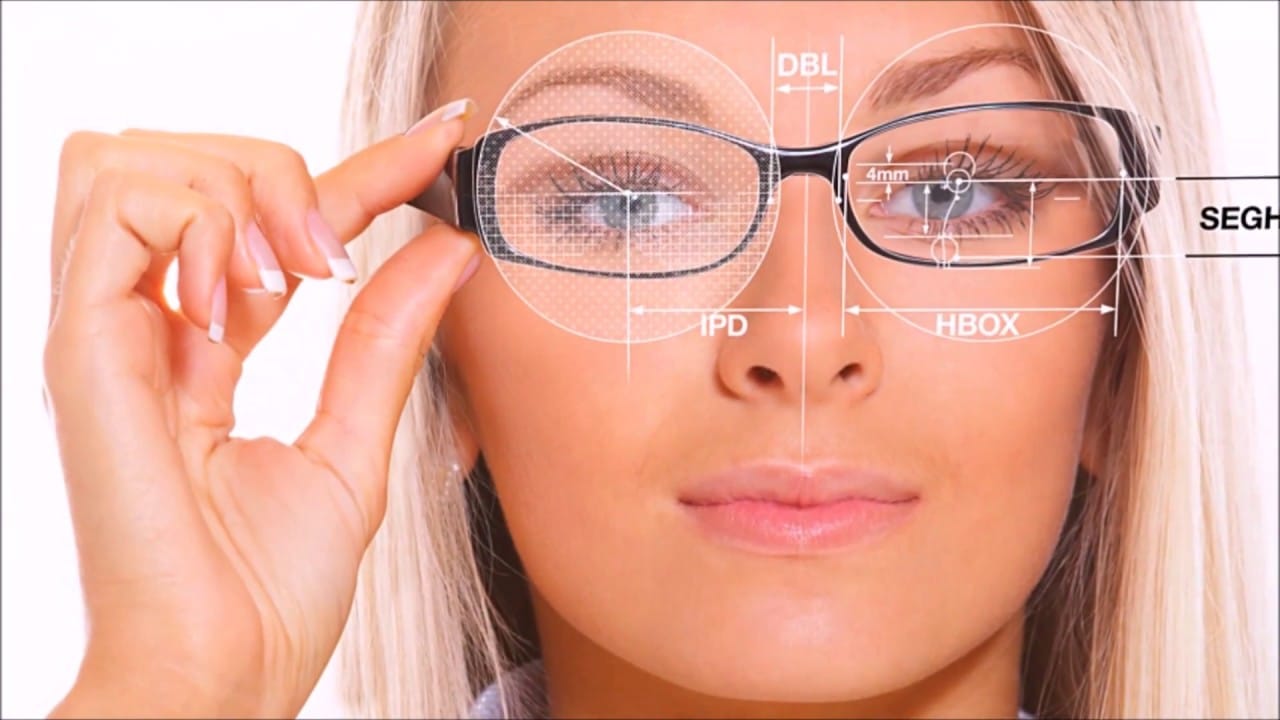
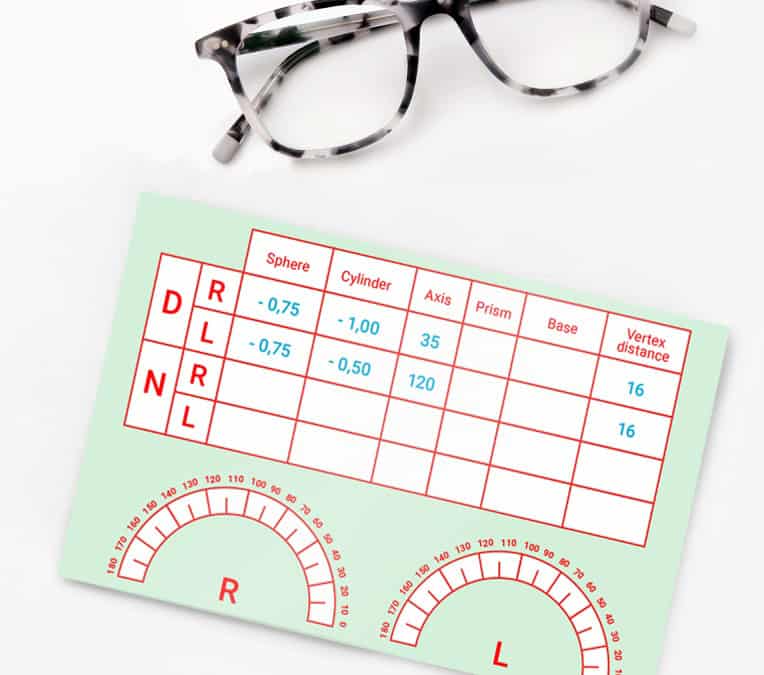
What is an eyeglass prescription?
An eyeglass prescription is a prescription written by a vision professional and authorizes a licensed optician to provide eyeglasses to you. An eyeglass prescription can be issued only by an optometrist or a physician, who may be an ophthalmologist. In Ontario, only optometrists, physicians and opticians are authorized to sell prescription eyeglasses. If the eye exam indicates that corrective lenses are necessary, the prescriber generally writes a prescription for an optical device. The parameters indicated on the prescription include the dioptric power of each lens to be made in order to correct the visual blur.
The prescription you are provided with by the optometrist is based on the information retrieved from your eye examination. In order to accurately determine how your vision can be corrected, the optometrist will consider:
- your overall health history, family history and your day to day visual demands
- how your eyes work together
- the general health of your eyes
- the lenses required for you to achieve the best vision and focus
Prescriptions given after an eye examination may vary from time to time depending on the measurements taken by the optometrist. Minor variations in the prescription are normal and may not affect the way you see.
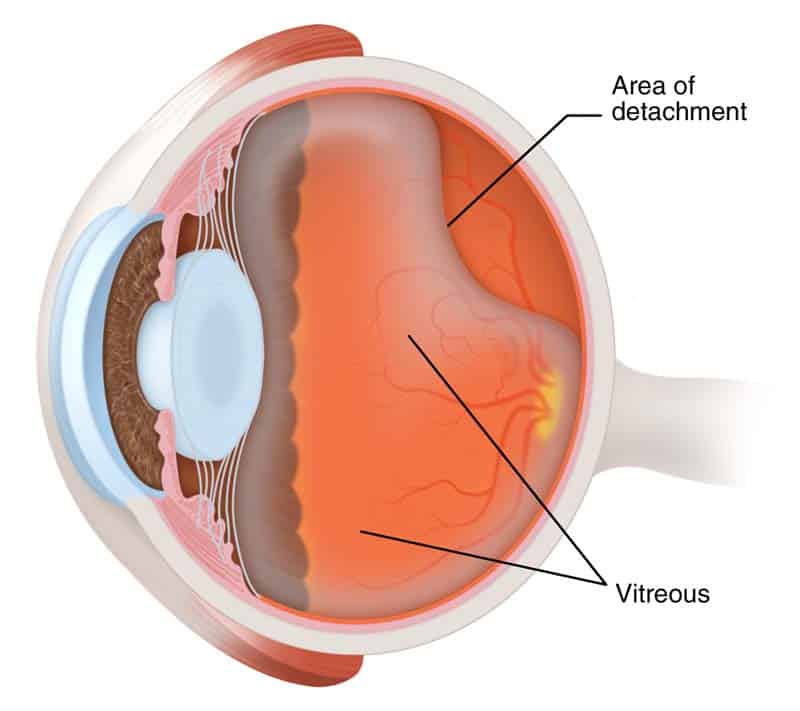
Retinal Detachment
Retinal Detachment?
Retinal detachment is an eye condition which involves separation of the retina from its attachments to the underlying tissue within the eye. This condition is a serious problem that usually affects middle-aged or older people. If it isn't treated immediately, it will lead to vision problems or even vision loss. Most retinal detachments are as a result of a retinal break, hole, or tear. These retinal breaks may occur when the vitreous gel separates from its attachment to the retina it usually happens in the peripheral parts of the retina. The vitreous is the clear gel that fills the space between the lens and the retina. The vitreous is attached to the retina in a few places. As we get older it separates and may tear the retina at those areas of attachment. Most retinal breaks are not a result of injury. Retinal tears are sometimes accompanied by bleeding. Many people develop separation of the vitreous from the retina as they get older. However, only a small percentage of these vitreous separations result in retinal tears. Having a yearly eye examination by optometrist helps to detect and treat retinal attachment
Nearsightedness, infection or injury such as a hard solid blow to the eye, can also make the vitreous separate. It is more common in people with a family history of retinal detachment. When there is a hole in the retina, fluid from the vitreous space may pass through the hole and flow between the retina and the back wall of the eye. This can separate the retina from the back of the eye and cause it to detach. The detached part of the retina will not work properly, and you will see a blurry or blind spot in your field of vision.
Less commonly, retinal detachment can also be caused by eye diseases, complications of diabetes, or tumours. In these cases there may be no tears or holes in the retina.
Retinal detachment facts:
- Most retinal detachments are a result of a retinal break, hole, or tear. Most retinal breaks, holes, or tears are not the result of trauma but are due to preexisting factors such as high levels of myopia, prior ocular surgery, and other eye diseases.
- Flashing lights and floaters may be the initial symptoms of a retinal detachment or of a retinal tear that precedes the detachment itself.
- Early diagnosis and repair of retinal detachments are important.
- The surgical repair of a retinal detachment is usually successful in reattaching the retina.
What is the retina?
The retina is an extremely thin tissue that lines the inside of the back of the eye. When we look around, light from directions enters in to the eye. The light image is focused onto the retina by both the cornea and the lens. This light striking the retina causes a complex biochemical change within layers of the retina. And this, in turn, stimulates an electrical response within other layers of the retina. Nerve endings within the retina transmit these electrical signals to the brain through the optic nerve. This electrical energy is received by brain and processed to allow us both to see and to understand what we are seeing. The retina, in contrast, continually renews itself chemically and electrically. And allowing us to see millions of different images every day without them being superimposed.
Risk factors of retinal detachment:
Research have shown that the incidence of retinal detachments caused by tears in the retina is very low. Affecting approximately one in 10,000 people every year. Many retinal tears do not progress to retinal detachment. Retinal detachments can occur at any age but are most common in adults 50 years and older. Specially those who are highly nearsighted or myopic and in older people following cataract surgery.
What other factors are associated with a retinal detachment?
- Blunt trauma, like penetrating injury by a sharp object to the eye can lead to a retinal detachment.
- A family history of a detached retina
- In some patients with a non-traumatic retinal detachment of one eye, a detachment subsequently occurs in the other eye. Accordingly, the second eye of a patient with a retinal detachment must be examined thoroughly every year, both by the patient and the ophthalmologist.
- Diabetes also can lead to a type of retinal detachment
- Non-rhegmatogenous retinal detachments is another kind. This kinds are not as a result of a retinal break, hole, or tear. These include conditions known as exudative retinal detachments and tractional retinal detachments.
How is Retinal Detachment Treated?
If the retina is torn, you may be able to stop detachment by receiving the tear treated quickly. If there is a little or no detachment at all, tears can sometimes be sealed with a laser. The laser makes small burns to seal the edges of the tear. This can be done without a hospital stay.
Freezing is another way of sealing the edges of the tear. But you will need a local anesthetic to numb the eye. No need to stay in hospital.
If the retina is detached, you will need surgery. In over 92% of cases, retinal detachment can be treated successfully. Sometimes, more than one operation is needed. Sometimes the ophthalmologist has to drain fluid so the retina can settle onto the back wall of the eye.
In more complicated cases, a procedure named a 'vitrectomy' is done. This involves cutting the vitreous away from the retina and taking it out of the eye. About 40% of people who have their detachment successfully repaired have excellent vision within 6 months of surgery. The results are not usually as good when the retina has been detached for a long time or when there is a fibrous growth on the surface of the retina. Please remember getting yearly eye examination by optometrist is very important.
Please click here for more info
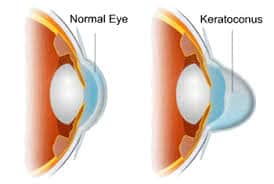
Keratoconus
Keratoconus is an eye disorder. Keratoconus causes cornea to thin, weaken and bulge forward. This distortion of cornea can result in poor vision, glare and difficulty with night time driving. The distortion of the cornea called irregular astigmatism as well. And results in poor vision and glare. The photos below are optical simulations of a patient with keratoconus.
Before 1998, the only treatment for patient with keratoconus was custom contact lenses, and Intacs or corneal transplants. Now patients have other non-invasive options which is highly effective with good safety records.
Cross linking is now being performed for patients. In the USA, Corneal Cross Linking is not yet widely available as this combination therapy with UV light and Vitamin eye drops (riboflavin) is not approved by the US Food and Drug Administration ("FDA").
Causes of Keratoconus
The cause of keratoconus is still unknown. Doctors have found that the disease often runs in families. It is important to get the eye exam done on a yearly basis for all family members of patients with keratoconus. Catching the disease early is critical and if the disease is caught early, it may be possible to prevent family members from developing poor vision.
Treatment options for Keratoconus
With the developments in technology and more research, treatment options have come a long way since it was first diagnosed.
In the early stages, eyeglasses or soft contacts will correct the corneal irregularity. Which presents itself in the form of nearsightedness and astigmatism.
Astigmatism is when the eye is oval shaped instead of being perfectly round. However, as the condition progresses, hard contact lenses are used to recreate a smooth front surface of the eye. Today, hybrid contact lenses that are soft on the outside and hard on the inside are used to improve vision. Hybrid contact lenses are very comfortable as opposed to previous treatment options.
However, treatment options do not stop there. The newest technology is larger. Scleral contact lenses require a lot of time and patience to maximize the fit and vision. Surgically, Intacts intracorneal rings, are an excellent treatment option. This Technic flatten the cornea. Another, newer treatment option called collagen cross-linking. This treatment is showing promise at slowing the progression of this disease. Especially in teenage patients. In severe cases, a corneal transplant may be needed due to extreme thinning and scarring of the cornea.
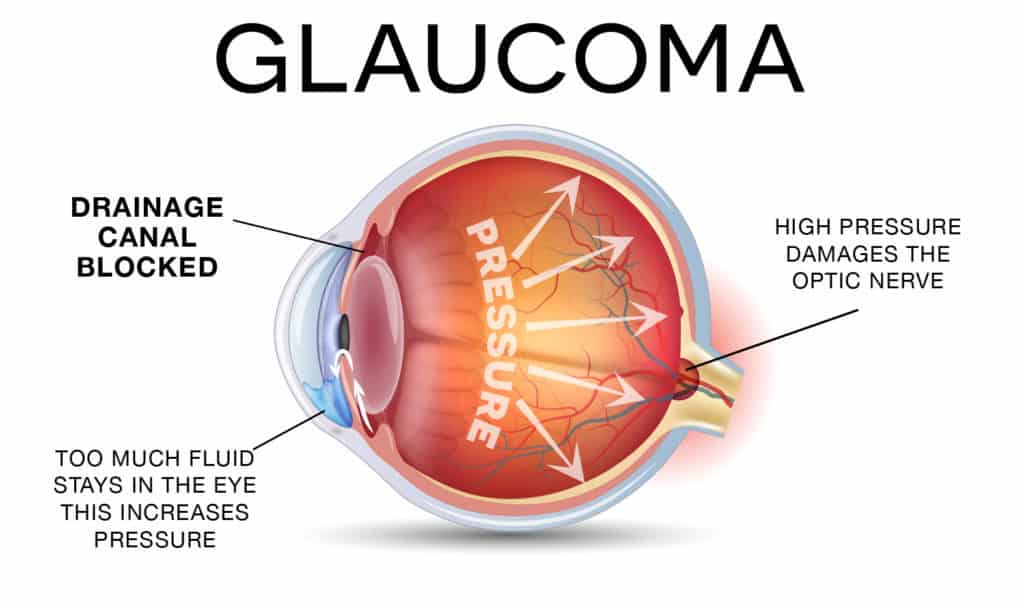
Glaucoma
Glaucoma is a disease that damages the optic nerve of your eye’s. Usually, it occurs when fluid builds up in the front part of your eye. That extra fluid accumulate in the front of your eyes, increases the pressure of eye, damaging the optic nerve. Glaucoma is a number one cause of blindness for people over 60 years old. But blindness from glaucoma can often be prevented with early treatment.
Types of glaucoma
There are two types of glaucoma.
- Open Angle Glaucoma
- Angle Closure Glaucoma
Open-Angle Glaucoma
Open angle is the most common type of glaucoma. This type of Glaucome happens slowly, where the eye does not drain fluid as well as it should and eye pressure builds up and starts damaging the optic nerve. This type of glaucoma is pain free and causes no vision changes at the beginning.
Regular eye examinations are very important to find early signs of damage to their optic nerve.
Angle-closure glaucoma
Angle closure glaucoma happens when patient’s iris is very close to the drainage angle in their eye. As a result iris can block the drainage angle. It is like when a piece of tissue or paper covers a sink drain. When the drainage angle gets completely blocked, eye pressure rises quickly. This is called an Acute Attack. It is very painful and It is a true eye emergency. In this case you should call your optometrist or ophthalmologist right away or you might go blind.
Here are the signs of an acute angle-closure glaucoma attack:
1. Blurry Vision
2. Severe eye pain
3. Headache
4. Nausea
5. Vomit
6. You see rainbow-colored rings or halos around lights
Fast facts on glaucoma:
1. Glaucoma has been called the silent thief of sight.
2. The main types of glaucoma are open-angle and closed-angle.
3. Age and thyroid problems increase the risk of glaucoma.
4. Symptoms can include severe eye pain.
5. Treatment includes surgery and medications.
Many people with angle-closure glaucoma develop it gradually and slowly. This is called chronic angle-closure glaucoma. There are no symptoms at first, so they don’t know they have it until the damage is severe or they have an attack.
Angle-closure glaucoma can cause blindness if not treated right away.
Having yearly eye examination is very important to detect any abnormality in your eyes.
To book an appointment, please call 905-832-6262 or send us an email to eyesoneyesoptical@yahoo.ca
Please click here for more info.