IMPORTANT CARE AND CLEANING TIPS FOR EYEGLASSES
Glasses can accumulate dirt, smudges and dust throughout the day. Regardless of how often you use your glasses, is important be proactive in order to keep them clean and to protect the lenses.
How to Clean Your Glasses
Before you start handling and cleaning your glasses, make sure to properly clean your hands in order to get rid of dirt, grime, and oils. Next, you must rinse the lenses with lukewarm water. Remember to not use hot water or any chemicals as this will cause the coatings of the lenses to dissipate over time. The safest solution to clean your lenses with is the spray cleaner that came with your glasses. You can also use a drop of liquid dish soap on your fingers to gently rub away the buildup on your lenses. Ensure you also wash the nose pads and frames with your solution aside from the lenses. Lastly to finish, give the glasses a final rinse in lukewarm water and thoroughly dry them with a lint-free cloth. During the day, make sure you carry a lint free cloth in your eye glasses case in order to touch up your glasses and maintain their cleanliness throughout the day so that you can consistently see clearly.
While cleaning your eye glasses is an easy task, there are a few common mistakes that you should avoid doing while cleaning your glasses.
Here are a few things that you should avoid:
It might seem more convenient to clean your lenses with the hem of your shirt as needed, but clothing can damage your eye glasses. The small pieces of dust or dirt on your shirt can scratch the lenses. Also, avoid using paper products such as napkins, paper towels or tissues as they carry dust.
Never use harsh cleaning products to clean your lenses as they could deteriorate or damage the coating on the lenses. For example, avoid using products such as ammonia based cleaners, window cleaner, bleach or vinegar. Lastly, if the water you are using to clean your lenses is too hot, it can damage certain types of coatings that have been applied to the lenses.
If you have questions about caring for your lenses and frames, then you can talk to our team for recommendations. To book an appointment for an eye exam to see an optometrist, please call us at 905-832-6262
Maple optometrist Location: 9929 Keele St, Unit 110, Maple, ON L6A 1Y5
The top 3 most common types of eye injuries and what to do If they happen to you
1- Corneal abrasion (Scratched Eye)
Some of the frequent causes of corneal abrasions are rubbing your eye with a foreign entity such as sand or dust, and getting poked in the eye. When a corneal abrasion happens, the patient will experience discomfort, redness in the eye, and sensitivity to light.
If suffering from a corneal abrasion or scratched eye, do not rub the eye or patch the eye. Putting an eye patch over the eye may create an ideal environment for fungus and other bacteria to grow, as fungus and bacteria strive and grow in cool, damp and dark places.
Seek professional medical care as soon as possible by going to your optometrist or the emergency room. At our Maple optometrist location, we have optometrist on premises.
2- Foreign Objects and/or Penetration in the eye
In the case that a foreign object such as shards of metal, or a piece of metal such as a fish hook enter your eye, seek professional medical attention right away. Do not attempt to remove or move the foreign object(s) in your eye under an circumstance as you will most likely cause more harm and damage to your eye.
The eye is a very sensitive area of the body. Cover the eye with an eye shield or you can loosely tape a paper cup over the eye for temporary protection until you reach a medical professional.
3- Chemical Burn in the Eye
Getting splashed in the eye with a liquid other than clean pure water can be frightening. In some circumstances, some substances can cause serious injury or permanent damage to the eye or your vision, while others may burn and sting but ultimately will not cause permanent damage. Depending on the chemical makeup of the substance that has entered your eye, the long term and short term effects can differ.
Acid: If acid has been splashed into your eye, you will experience instant redness and burning but can be washed out pretty easily
Alkali: If splashed in the eye with an alkali substance, you will not feel as much irritation, burning, or redness as an acid, but they are far more dangerous.
Examples of alkali substances are toilet bowl cleaners, chalk dust, and oven cleaners.
Chemical exposure to the eye is usually caused by the chemical being splashed into the eye, rubbing your eye and transferring them chemical
from your hand to your eye, or by getting sprayed in the eye with an aerosol or spray bottle.
If ever splashed in the eye with a chemical, place your head under a stream of lukewarm water and let the water run gently into your eye and down your face for 15 minutes. Ensure you contact an eye care professional as soon as possible or go to an emergency clinic to receive medical attention.
If you have questions, you can talk to our team for recommendations. We sell the best lenses and coatings in our Maple Location. To book an appointment for an eye exam to see an optometrist, call us at 905-832-6262.
Please click here for more info
Our Maple optometrist Location:
Eyes on Eyes Optical
9929 Keele St, Unit 110, Maple, ON L6A 1Y5, Tel: 905-832-6262
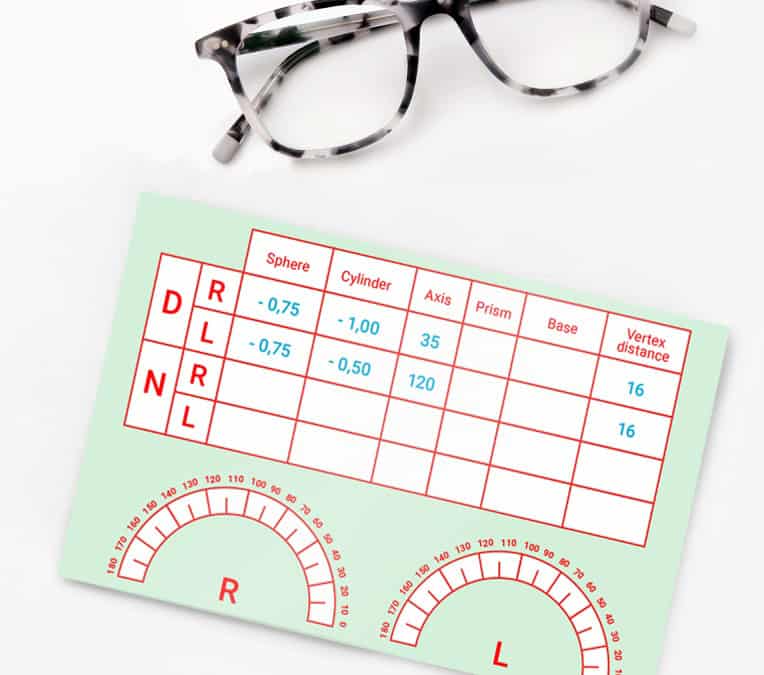
What is an eyeglass prescription?
An eyeglass prescription is a prescription written by a vision professional and authorizes a licensed optician to provide eyeglasses to you. An eyeglass prescription can be issued only by an optometrist or a physician, who may be an ophthalmologist. In Ontario, only optometrists, physicians and opticians are authorized to sell prescription eyeglasses. If the eye exam indicates that corrective lenses are necessary, the prescriber generally writes a prescription for an optical device. The parameters indicated on the prescription include the dioptric power of each lens to be made in order to correct the visual blur.
The prescription you are provided with by the optometrist is based on the information retrieved from your eye examination. In order to accurately determine how your vision can be corrected, the optometrist will consider:
- your overall health history, family history and your day to day visual demands
- how your eyes work together
- the general health of your eyes
- the lenses required for you to achieve the best vision and focus
Prescriptions given after an eye examination may vary from time to time depending on the measurements taken by the optometrist. Minor variations in the prescription are normal and may not affect the way you see.
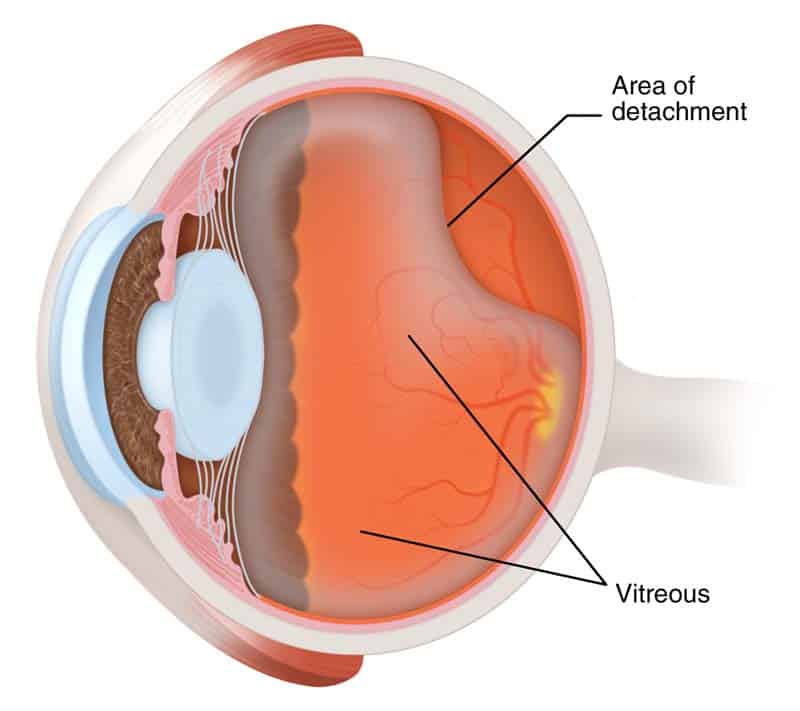
Retinal Detachment
Retinal Detachment?
Retinal detachment is an eye condition which involves separation of the retina from its attachments to the underlying tissue within the eye. This condition is a serious problem that usually affects middle-aged or older people. If it isn't treated immediately, it will lead to vision problems or even vision loss. Most retinal detachments are as a result of a retinal break, hole, or tear. These retinal breaks may occur when the vitreous gel separates from its attachment to the retina it usually happens in the peripheral parts of the retina. The vitreous is the clear gel that fills the space between the lens and the retina. The vitreous is attached to the retina in a few places. As we get older it separates and may tear the retina at those areas of attachment. Most retinal breaks are not a result of injury. Retinal tears are sometimes accompanied by bleeding. Many people develop separation of the vitreous from the retina as they get older. However, only a small percentage of these vitreous separations result in retinal tears. Having a yearly eye examination by optometrist helps to detect and treat retinal attachment
Nearsightedness, infection or injury such as a hard solid blow to the eye, can also make the vitreous separate. It is more common in people with a family history of retinal detachment. When there is a hole in the retina, fluid from the vitreous space may pass through the hole and flow between the retina and the back wall of the eye. This can separate the retina from the back of the eye and cause it to detach. The detached part of the retina will not work properly, and you will see a blurry or blind spot in your field of vision.
Less commonly, retinal detachment can also be caused by eye diseases, complications of diabetes, or tumours. In these cases there may be no tears or holes in the retina.
Retinal detachment facts:
- Most retinal detachments are a result of a retinal break, hole, or tear. Most retinal breaks, holes, or tears are not the result of trauma but are due to preexisting factors such as high levels of myopia, prior ocular surgery, and other eye diseases.
- Flashing lights and floaters may be the initial symptoms of a retinal detachment or of a retinal tear that precedes the detachment itself.
- Early diagnosis and repair of retinal detachments are important.
- The surgical repair of a retinal detachment is usually successful in reattaching the retina.
What is the retina?
The retina is an extremely thin tissue that lines the inside of the back of the eye. When we look around, light from directions enters in to the eye. The light image is focused onto the retina by both the cornea and the lens. This light striking the retina causes a complex biochemical change within layers of the retina. And this, in turn, stimulates an electrical response within other layers of the retina. Nerve endings within the retina transmit these electrical signals to the brain through the optic nerve. This electrical energy is received by brain and processed to allow us both to see and to understand what we are seeing. The retina, in contrast, continually renews itself chemically and electrically. And allowing us to see millions of different images every day without them being superimposed.
Risk factors of retinal detachment:
Research have shown that the incidence of retinal detachments caused by tears in the retina is very low. Affecting approximately one in 10,000 people every year. Many retinal tears do not progress to retinal detachment. Retinal detachments can occur at any age but are most common in adults 50 years and older. Specially those who are highly nearsighted or myopic and in older people following cataract surgery.
What other factors are associated with a retinal detachment?
- Blunt trauma, like penetrating injury by a sharp object to the eye can lead to a retinal detachment.
- A family history of a detached retina
- In some patients with a non-traumatic retinal detachment of one eye, a detachment subsequently occurs in the other eye. Accordingly, the second eye of a patient with a retinal detachment must be examined thoroughly every year, both by the patient and the ophthalmologist.
- Diabetes also can lead to a type of retinal detachment
- Non-rhegmatogenous retinal detachments is another kind. This kinds are not as a result of a retinal break, hole, or tear. These include conditions known as exudative retinal detachments and tractional retinal detachments.
How is Retinal Detachment Treated?
If the retina is torn, you may be able to stop detachment by receiving the tear treated quickly. If there is a little or no detachment at all, tears can sometimes be sealed with a laser. The laser makes small burns to seal the edges of the tear. This can be done without a hospital stay.
Freezing is another way of sealing the edges of the tear. But you will need a local anesthetic to numb the eye. No need to stay in hospital.
If the retina is detached, you will need surgery. In over 92% of cases, retinal detachment can be treated successfully. Sometimes, more than one operation is needed. Sometimes the ophthalmologist has to drain fluid so the retina can settle onto the back wall of the eye.
In more complicated cases, a procedure named a 'vitrectomy' is done. This involves cutting the vitreous away from the retina and taking it out of the eye. About 40% of people who have their detachment successfully repaired have excellent vision within 6 months of surgery. The results are not usually as good when the retina has been detached for a long time or when there is a fibrous growth on the surface of the retina. Please remember getting yearly eye examination by optometrist is very important.
Please click here for more info
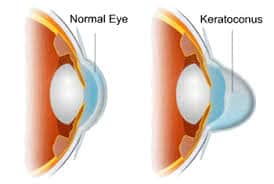
Keratoconus
Keratoconus is an eye disorder. Keratoconus causes cornea to thin, weaken and bulge forward. This distortion of cornea can result in poor vision, glare and difficulty with night time driving. The distortion of the cornea called irregular astigmatism as well. And results in poor vision and glare. The photos below are optical simulations of a patient with keratoconus.
Before 1998, the only treatment for patient with keratoconus was custom contact lenses, and Intacs or corneal transplants. Now patients have other non-invasive options which is highly effective with good safety records.
Cross linking is now being performed for patients. In the USA, Corneal Cross Linking is not yet widely available as this combination therapy with UV light and Vitamin eye drops (riboflavin) is not approved by the US Food and Drug Administration ("FDA").
Causes of Keratoconus
The cause of keratoconus is still unknown. Doctors have found that the disease often runs in families. It is important to get the eye exam done on a yearly basis for all family members of patients with keratoconus. Catching the disease early is critical and if the disease is caught early, it may be possible to prevent family members from developing poor vision.
Treatment options for Keratoconus
With the developments in technology and more research, treatment options have come a long way since it was first diagnosed.
In the early stages, eyeglasses or soft contacts will correct the corneal irregularity. Which presents itself in the form of nearsightedness and astigmatism.
Astigmatism is when the eye is oval shaped instead of being perfectly round. However, as the condition progresses, hard contact lenses are used to recreate a smooth front surface of the eye. Today, hybrid contact lenses that are soft on the outside and hard on the inside are used to improve vision. Hybrid contact lenses are very comfortable as opposed to previous treatment options.
However, treatment options do not stop there. The newest technology is larger. Scleral contact lenses require a lot of time and patience to maximize the fit and vision. Surgically, Intacts intracorneal rings, are an excellent treatment option. This Technic flatten the cornea. Another, newer treatment option called collagen cross-linking. This treatment is showing promise at slowing the progression of this disease. Especially in teenage patients. In severe cases, a corneal transplant may be needed due to extreme thinning and scarring of the cornea.
Glaucoma
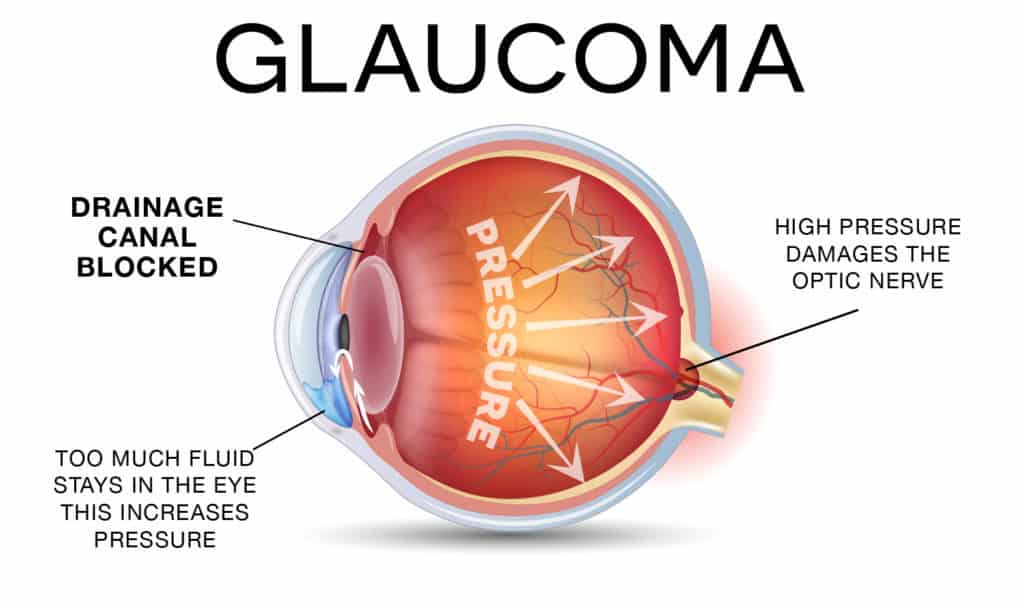
Glaucoma is a disease that damages the optic nerve of your eye’s. Usually, it occurs when fluid builds up in the front part of your eye. That extra fluid accumulate in the front of your eyes, increases the pressure of eye, damaging the optic nerve. Glaucoma is a number one cause of blindness for people over 60 years old. But blindness from glaucoma can often be prevented with early treatment.
Types of glaucoma
There are two types of glaucoma.
- Open Angle Glaucoma
- Angle Closure Glaucoma
Open-Angle Glaucoma
Open angle is the most common type of glaucoma. This type of Glaucome happens slowly, where the eye does not drain fluid as well as it should and eye pressure builds up and starts damaging the optic nerve. This type of glaucoma is pain free and causes no vision changes at the beginning.
Regular eye examinations are very important to find early signs of damage to their optic nerve.
Angle-closure glaucoma
Angle closure glaucoma happens when patient’s iris is very close to the drainage angle in their eye. As a result iris can block the drainage angle. It is like when a piece of tissue or paper covers a sink drain. When the drainage angle gets completely blocked, eye pressure rises quickly. This is called an Acute Attack. It is very painful and It is a true eye emergency. In this case you should call your optometrist or ophthalmologist right away or you might go blind.
Here are the signs of an acute angle-closure glaucoma attack:
1. Blurry Vision
2. Severe eye pain
3. Headache
4. Nausea
5. Vomit
6. You see rainbow-colored rings or halos around lights
Fast facts on glaucoma:
1. Glaucoma has been called the silent thief of sight.
2. The main types of glaucoma are open-angle and closed-angle.
3. Age and thyroid problems increase the risk of glaucoma.
4. Symptoms can include severe eye pain.
5. Treatment includes surgery and medications.
Many people with angle-closure glaucoma develop it gradually and slowly. This is called chronic angle-closure glaucoma. There are no symptoms at first, so they don’t know they have it until the damage is severe or they have an attack.
Angle-closure glaucoma can cause blindness if not treated right away.
Having yearly eye examination is very important to detect any abnormality in your eyes.
To book an appointment, please call 905-832-6262 or send us an email to eyesoneyesoptical@yahoo.ca
Please click here for more info.
Lazy Eye
Lazy eye is an early childhood condition in which a child's eyesight does not develop as it should in one eye. Lazy eye is also known as Amblyopia.
When a child has lazy eye, the brain only focuses on a good eye more than the other, practically ignoring the lazy eye. If that eye is not activated properly, the nerve cells responsible for vision do not mature normally.
Lazy eye affects approximately %2 of all children in north of America. Lazy eye is the most common cause of partial or total blindness in one eye.
- Lazy eye is not a problem with the eye. The term "lazy eye" is misleading because the eye is not lazy. In fact, it is a developmental problem in the nerve connecting the eye to the brain, not a problem in the eye itself. Lazy eye can be caused by a number of factors, including a muscle imbalance or eye disease. Cure can be effective if it begins earlier when child is younger.
- Symptoms of lazy eye includes blurred vision and poor depth perception. After child is 8 years of age, vision improvement drops somewhat but still can be effective.
- Many children who have unequal vision, or an isometropia, do not know they have an eye problem because the stronger eye and the brain compensate for the shortfall. The weaker eye gets progressively worse, and amblyopia develops.
- A child with near-sightedness, far-sightedness, or astigmatism will be prescribed glasses. The child with Lazy eye have to wear spectacle at all the time so that the specialist can monitor how effective they are at improving the vision problems. Spectacles may also correct an eye turn. Sometimes, glasses can solve the lazy eye, and no more treatment is required.
How to Fix Lazy Eye or Amblyopia
Early treatment of lazy eye is usually easy with wearing eyeglasses, vision therapy, Atropine drops, eye patching. Detection and correction before the age of two or at younger age is considered to get the best result. Neuroscience has proven that the human brain can change at any age, so lazy eye is treatable at any age. Studies on neuroplasticity of the brain in adults are now showing that therapies can improve the vision in lazy eye conditions in older children and adults.
Treatment of amblyopia after the age of 17 is not dependent upon age but requires more effort including vision therapy. Every patient with lazy eye deserves an attempt at treatment.
Exercises help to correct vision. Usually the stronger eye may be patched, and the weaker eye stimulated with a range of vision-intensive activities, such as coloring, dot-to-dot drawing, word games, or building Lego, depending on the age of the child. People with Lazy eye, recommend to do an eye exam every year with optometrist or Ophthomologist. Eye examination for people with lazy eye is covered by Ohip.
Dry Eye and How to Deal With It
What is Dry Eye?
Dry eyes is a very common and every day condition. Dry eye happens when your tears aren’t able to produce enough and adequate lubrication for your eyes. Tears can be insufficient for many reasons. Tears are a mixed up of water, fatty oils and mucus. This mixture assists make the surface of your eyes fluidly and clear, and it helps defend and secure your eyes from infection.
For instance, dry eyes may occur if your eyes produce enough tears or if you produce less amount of tears.
Dry eyes feels very annoying and troublesome. When you have dry eyes, your eyes may sting or burn. You may experience dry eyes in different situations, like when you are on computer for long hours, or when you are on an airplane.
Many times , we will experience a “foreign body sensation” in our eye. That usually happens if the wind blows dust, an allergen or a foreign body into our eye or under an eyelid. This should not be dismissed as just an uncomfortable feeling. It needs to be remedied. It cannot be allowed to linger or fester.
Dry eye syndromes
For many, the feeling of grittiness, dryness, burning or stinging or even excessive tearing cannot be relieved simply, or with over the counter methods. It may be the sign of a chronic condition known as dry eye syndrome. Yes, even tearing eyes are a sign of dry eye.
The tears your eyes produce are necessary for overall eye health and clear vision. Dry eye means that your eyes do not produce enough tears or that you produce tears that do not have the proper chemical composition.
Dry eye is more common as we age. It can also be caused by blinking or eyelid problems, medications like antihistamines, oral contraceptives and antidepressants, a dry climate, wind and dust, general health problems like arthritis or Sjogren’s syndrome and chemical or thermal burns to your eyes. If you have dry eye, visit your optometrist for treatment.
If you have dry eye, your symptoms may include irritated, scratchy, dry, uncomfortable or red eyes, a burning sensation, excessive tearing, blurred vision, or a feeling of something foreign in your eyes. Excessive dry eyes may damage eye tissue, scar your cornea (the front covering of your eyes) and impair vision and make contact lens wear difficult.
Careful clinical observation, accurate diagnosis, and appropriate intervention can eliminate or minimize the deleterious effects of ocular surface disorders on the quality of life.
For more info please click here.